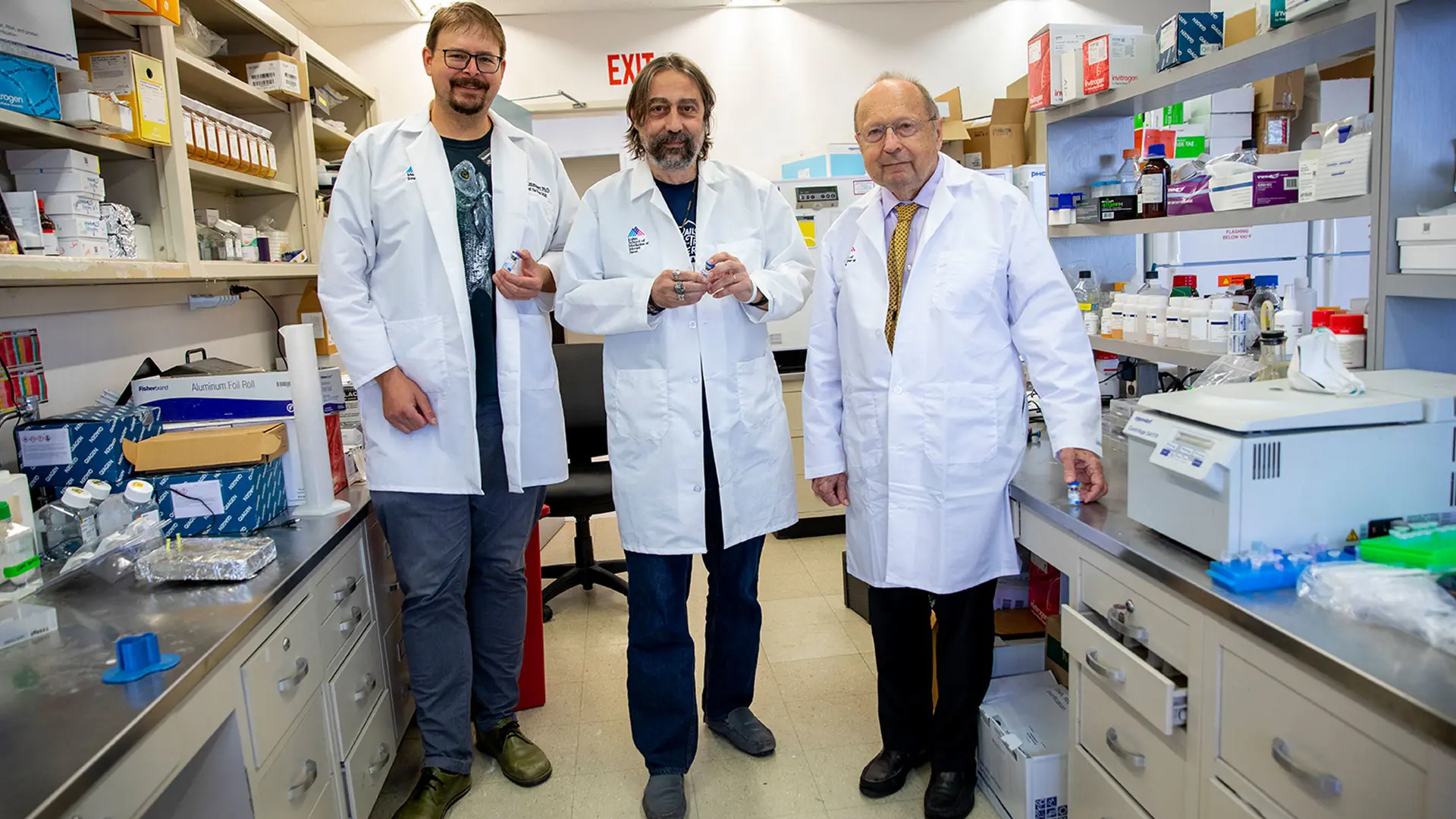
Mount Sinai's leading vaccine developers, from left, Florian Krammer, PhD; Adolfo Garcia-Sastre, PhD; and Peter Palese, PhD.
The development of a safe, effective, and inexpensive COVID-19 vaccine that can easily be produced and distributed in low- and-middle-income countries is underway at the Icahn School of Medicine at Mount Sinai, where early phase 1 clinical testing in Vietnam and Thailand has shown positive results.
The vaccine is the brainchild of three renowned scientists at Mount Sinai—Peter Palese, PhD, Horace W. Goldsmith Professor and Chair of the Department of Microbiology; Adolfo García-Sastre, PhD, Irene and Dr. Arthur M. Fishberg Professor of Medicine and Director of the Global Health and Emerging Pathogens Institute; and Florian Krammer, PhD, Mount Sinai Professor in Vaccinology. By combining their expertise, the scientists—who previously developed a universal influenza vaccine—hope to bring closure to this deadly pandemic by providing less affluent countries with an accessible and cost-effective COVID-19 vaccine they can manufacture themselves.
To date, COVAX, a global collaboration that includes the World Health Organization, has shipped more than 95 million vaccines to 134 countries, far short of the number needed to stop the spread of SARS-CoV-2, the virus that leads to COVID-19. More contagious variants of the virus will continue to evolve and plague countries around the world as long as their populations remain unvaccinated. “When we protect other countries we protect ourselves, as well,” says Dr. Palese.
Dr. Krammer says, “In North America and Europe many people are getting vaccinated and the virus circulation is going down. But that is not the case in countries in Asia or Latin America, for example. Their COVID-19 case numbers are going up quickly. They need a vaccine and they don’t have access.”
Anticipating this need, Dr. Palese and his colleagues designed Mount Sinai’s COVID-19 vaccine to use the avian Newcastle virus (NDV), and constructed it similarly to an influenza virus vaccine, which can be manufactured in embryonated or fertilized chicken eggs.
The vaccine is stable and highly immunogenic.
The NDV-based vaccine is engineered to express the spike protein of SARS-CoV-2. The construct is injected into an embryonated egg, the virus replicates, and the amplified vaccine virus is then collected, purified, and inactivated. According to Dr. Palese, the resulting vaccine is stable, extraordinarily immunogenic, and induces highly protective immune responses against SARS-CoV-2. Immunogenicity is a measure of the type of immune responses that a vaccine generates and their magnitude over time.
“The beauty of this vaccine is that it can be made using the same influenza vaccine production facilities that many countries already have” in place, Dr. Krammer says. Approximately three billion doses of flu vaccine are produced each year using embryonated eggs.
There are other advantages, as well. Mount Sinai’s Newcastle vector vaccine does not appear to cause any side effects, such as the low-grade fevers, headaches, or pain and swelling at the injection site that are associated with the Moderna and Pfizer-BioNTech mRNA vaccines. The vaccine can also be stored at the same temperature as a home refrigerator, whereas both mRNA vaccines require extra-cold temperatures found only in commercial-grade freezers.
Mount Sinai’s vaccine, says Dr. Palese, can “probably be produced for under one dollar per dose,” and will require two doses spread over 21 days. By comparison, the mRNA vaccines, which also require two doses spread over three to four weeks, cost roughly $50 per dose. To keep costs down, Mount Sinai has agreed to grant licenses for its intellectual property to low- and middle-income countries that produce the vaccine and forgo any royalties on its use.
Dr. Garcia-Sastre says, “Prior to COVID-19, we realized the potential of NDV-based vaccines and for several years optimized this vaccine vector to achieve optimal immunogenicity of the delivered antigen (or toxin). NDV-based vaccines not only have the potential to stop COVID-19 in countries that have no access to the existing SARS-CoV-2 vaccines, but could be
easily tailored to stop future pandemics caused by novel pathogens.”
"Prior to COVID-19, we realized the potential of NDV-based vaccines."
As phase 2 testing for the vaccine ramps up in Thailand and Vietnam, accelerated phase 1 trials are ongoing in Mexico and Brazil. The trial designs used in these countries should lead to rapid phase 3 results. So far, the scientists say they have been pleased with their phase 1 results and with the tests that have been conducted in animal models.
“You can say that in animals, the vaccine protects beautifully,” says Dr. Krammer. “There is preliminary immunogenicity data that suggests the vaccine induces very good neutralizing titers.”
It is not yet clear whether the current vaccine will need to be updated to protect against aggressive new variants, according to Dr. Krammer. “But if it’s needed, we can change and move quickly to a variant vaccine. It would not be complicated.”
With regard to safety, which is top priority in a phase 1 trial, Dr. Palese says, “We are passing with flying colors.”
Featured
Dennis S. Charney, MD
Icahn Mount Sinai